NCDMod: A microsimulation model projecting chronic disease and risk factors for Australian adults
Abstract
Chronic disease and the associated risk factors are an ongoing public health concern. They represent a major burden of disease and result in significant health expenditure. The purpose of this paper is to describe the development and attributes of the microsimulation model NCDMod, an Australian, purpose-built model that simulates multiple chronic diseases and associated risk factors. The model offers flexibility in perspective and population of interest. The model projects out to 2025 in 5-year increments using a combination of static and dynamic methods. Transition equations are sourced from the literature and in-house analysis. NCDMod is able to capture the impacts of population ageing and shifts in incidence of specific chronic diseases and risk factors. Results from NCDMod will help to fill gaps in current Australian evidence on the population level impacts of interventions to prevent/delay chronic health conditions particularly diabetes, heart disease and obesity. Further, in combination with Health&WealthMod2030 this model will be able to offer evidence regarding the potential impact of health interventions on the long-term costs (both from an individual and government perspective) of ill health leading to unplanned retirement. In the consideration of disease interventions, the additional workers who may be able to continue to work due to delayed/prevented chronic disease can be modelled.
1. Introduction
Chronic diseases and their associated risk factors are major public health and policy concerns. There is a strong association between chronic disease, morbidity and mortality. The rate and absolute numbers of people with chronic diseases have been increasing providing health policy challenges especially related to expenditure on health care. Some 85 per cent of total burden of disease (BoD) was non-communicable (largely chronic) diseases in the Australasia region in 2010 (Australian Institute of Health and Welfare, 2014a). In 2011–12, 4.6% of Australians aged 2 years and over (999,000 people) had diagnosed diabetes (excluding gestational diabetes)(Australian Bureau of Statistics, 2013a), about 0.6% of persons had type 1 diabetes with the remaining 3.9% having type 2 diabetes. The age-standardised proportion of the Australian population with diabetes has increased across the 10 years between 2001 and 2011–12 from 3.4% to 4.4%. In 2011–12, 5.0% of Australians aged 2 years and over (1.1 million people) had heart disease, which included ischaemic heart disease (IHD), cerebrovascular disease, oedema, heart failure, and diseases of the arteries, arterioles and capillaries (Australian Bureau of Statistics, 2013a). Between 2001 and 2011–12 there was a shift in the age-standardised rates of heart, stroke and vascular disease from 4.4% to 4.7%. For Australian males in 2003, the two leading causes of disease burden was ischaemic heart disease with 151,107 disability adjusted life years (DALYs) at 11.1% of BoD followed by type 2 diabetes with 71,176 DALYs at 5.2% of BoD. For Australian women, IHD (112,390 DALYs at 8.9%) and type 2 diabetes (61,763 DALYs at 4.9%) were ranked second and fourth respectively (Begg et al., 2007).
Chronic disease is associated with significant health care expenditure. In 2008–09, it was reported that $AU7,605 million was spent on cardiovascular disease (CVD), approximately 12% of all health care expenditure in Australia. This was the largest single spend on a disease group (Australian Institute of Health and Welfare, 2014b). Similarly, diabetes is associated with considerable medical expenditure – in 2005 it was estimated that in 2010 $AU6.1 billion was spent on persons with known type 2 diabetes (Lee et al., 2013). Diabetes is associated with sizable economic impacts to both individuals and government in terms of lost income, decreased taxation revenue, increased government support payments and reduced savings at age 65 due to premature exit from the labour force because of diabetes. Those with diabetes have immediate limitation of income available, as well as reduced long-term financial capacity due to reduced accumulated savings and the income these savings could generate in retirement (Schofield et al., 2015). Similar findings have been reported for those with CVD (Schofield et al., 2012).
These two disease groups (diabetes and CVD) have a strong interrelationship particularly through their shared behavioural risk factors such as smoking and physical activity (Australian Institute of Health and Welfare, 2014a). As well, there are strong links between these chronic diseases and obesity (Australian Institute of Health and Welfare, 2015a). Considerable health burden is related to obesity both directly and via co-morbidities such as diabetes and CVD. In turn, this has large impacts on health expenditure and more widely on productivity. A systematic review which compared obese individuals with normal weight persons reported significant associations between obesity and all cancers, all CVDs, type 2 diabetes, asthma, gallbladder disease, osteoarthritis, and chronic back pain (Guh et al., 2009). The strength of association was strongest for type 2 diabetes with incidence rate ratios of 6.74 (95% confidence intervals: 5.55, 8.19) for men and 12.41 (95% confidence intervals: 9.03, 17.06) for women. Obesity is associated with impaired quality of life, increasing need for health care and medication spending, and substantial health care costs for obesity and related co-morbidities (Buchmueller & Johar, 2015; PwC, 2015; Withrow & Alter, 2011; World Health Organization, 2000).
With the significant disease burden, rising health expenditure, limited budgets and need for governments’ fiscal sustainability, cost-effectiveness models to evaluate prevention options, screening and new treatments are of prime importance. Simulation models can assist decision and cost-effectiveness analysis by facilitating the synthesis of information from several sources into a single comprehensive structure. Microsimulation modelling takes a bottom up simulation approach by modelling at the individual level. It then allows aggregation to consider population and sub-population level outcomes.
Internationally there are a number of disease-specific models available for diabetes aimed at life course outcomes for the diabetic population (Palmer, 2013) and/or CVD including myocardial infarct and/or stroke (Laditka & Laditka, 2014; Smolen et al., 2007). The UK (United Kingdom) Prospective Diabetes Study (UKPDS) outcomes model versions 1 and 2 offer simulation modelling (probabilistic discrete–time) to forecast occurrence of diabetes related complications and death. The model calculates the BoD over a population’s lifetime based on life expectancy, quality adjusted life years, complication rates and costs for each member of the population. The probability equations are based on the UKPDS (Clarke et al., 2004; Hayes, Leal, Gray, Holman, & Clarke, 2013). HealthAgeingMod, a disease specific model was developed for the Australian context, using a model-system framework that could track individual risk factors over time, model the incidence of heart disease, stroke and diabetes, estimate treatment costs and scale these impacts to an Australian level to estimate cost-benefits of policy reform. It was used to assess the impacts of population ageing and decreased obesity rates (Walker , Butler, & Colagiuri, 2013). From the UK, FORESIGHT is a model that has been used to simulate projected implications of various BMI (body mass index) reductions on 13 diseases and their future health costs (McPherson, Marsh, Rtveladze, Webber, & Brown, 2012). POHEM-CVD is a dynamic microsimulation model developed to reflect the individual’s lifecourse projecting their CVD related risk factors. It creates a synthetic population and ages each individual one at a time through to their death. It allows projection of disease incidence, prevalence, life expectancy, health adjusted life expectancy and quality of life (Manuel et al., 2014). This model is part of the broader POHEM modelling program which allows consideration of multiple diseases. Some microsimulation models have taken a broader view of chronic disease within the socio-economic context. However, these models often define health in a broader manner such as presence of disability, see for example MOSART (Fredriksen, 1998), CAPP_DYN (Mazzaferro & Morciano, 2008), INAHSIM-II (Fukawa, 2012) and/or a health status index as seen in INAHSIM-II (Fukawa, 2012) and SESIM LEV 2012 (Brouwers et al., 2014). The main purpose for these models are projections of social security expenditure (pre-dominantly disability and aged pensions) though some do consider health care expenditure, for example SESIM LEV (Brouwers et al., 2014). The predominant motivation in the development of these models is concern about the ageing population being experienced by developed countries. For example APPSIM, an Australian dynamic microsimulation model was developed to project socio-economic conditions over a 50 year period. This model included health as an index to allow projection of health care spending and disability status (Lymer, 2011). It did not model specific diseases in the population and associated impacts on life expectancy or quality adjusted life years. A more inclusive, general microsimulation model, SESIM is a Swedish dynamic microsimulation model that projects from 1999 to 2050. It is based on LINDA, a database of approximately 3.5% of the Swedish population. The model assigns baseline health status (4-point index from severe illness to full health) and health care consumption. Health status and health care consumption is then projected across time. In addition, specific disease and care consumption across time was separately modelled for diabetes, stroke, acute myocardial infarction (AMI) and cancer (Brouwers et al., 2014). In 2013, the redevelopment of HealthAgeingMod into NCDMod was the revision to an upgraded microsimulation model to dynamically model specific diseases (currently focusing on type 2 diabetes and CVD), their impacts on life expectancy, quality of life and costs of health care. The chronic diseases are linked to key risk factors, such as obesity, through the transition equations. The model now commences projections from a base year of 2010 and represents the Australian population at that time point. The focus has moved to the working age population and transition from early adulthood into middle age. This model provides the means to model cost-effectiveness at a population level for randomized clinical trials not previously available in HealthAgeingMod, as well as the capacity to consider counterfactual scenarios around health policy interventions. The current model can consider population level cost-effectiveness of prevention/interventions focussed on multifactorial risk factors such as obesity as well as intervention level cost-consequences.
This paper describes the development of the microsimulation model, NCDMod, which is a major redevelopment of HealthAgingMod (Walker et al., 2013). HealthAgeingMod was developed to project co-morbidity of chronic disease amongst the ageing Australian population and facilitate economic analysis of interventions to delay chronic disease (Walker et al., 2013). Further detail of NCDMod can be found in publications by Walker and others (Walker, Butler, & Colagiuri, 2011; Walker et al., 2013). NCDMod is an Australian, purpose-built model that simulates multiple diseases making use of the most current Australian data available. It utilises improved and updated transition equations from the previous modelling of HealthAgeingMod. The model offers greater flexibility in the perspectives it can consider which includes cost-effectiveness related to clinical trials, population health and policy interventions. Further, it allows analysis at intervention and population level as well as key sub-population analysis of interest such as high risk groups.
Using NCDMod, we will be able to undertake medium term projections from 2010 to 2025 of:
Impacts of demographic changes;
Impacts of effective interventions to address health risk factors; and
Impacts of effective interventions to address these health conditions at both an intervention and population level.
Further, with linkage to Health&WealthMod 2030, the modelling facilitates productivity projections for adults aged 45–65 years considering the impacts of effective interventions addressing risk factors and/or chronic disease.
2. Methods
NCDMod is a hydrid static-dynamic microsimulation model designed to simulate incidence and prevalence of key diseases and risk factors, as well as health care costs of Australians aged 20 years and over from 2010 to 2025. All of the model code and simulations have been written and run in SAS v9.4 software. Copyright© 2002–2012 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
The output data files of NCDMod consist of four datasets providing similar information on Australians aged 20 years and over but at different points in time (2010, 2015, 2020 and 2025). Each file includes data on the individuals’ demographics, risk factors, disease profile and cost of health care.
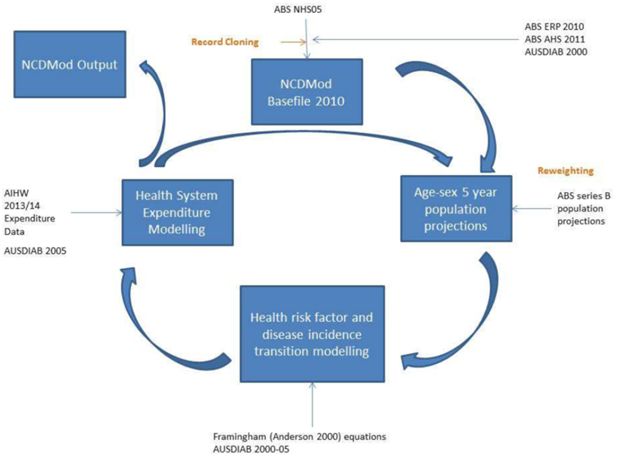
NCDMod has four main components: i) the base population – the microdata on which the model is built; ii) incidence models for chronic disease and risk factors; iii) health expenditure modelling; and iv) population projections from the Australian Bureau of Statistics (ABS). Figure 1 shows the schematic diagram of NCDMod and how each component is linked, with Table 1 outlining the key variables.
Summary of NCDMod key variables.
| Model Module | Variable |
|---|---|
| NCDMod Basefile | |
| Demography | Age
Sex Ethnicity Family type Socio-economic status |
| Chronic Illness | Diabetes
Cardiovascular disease Peripheral vascular disease Arthritis Cancer Asthma Renal failure Depression Dementia |
| Risk Factors | BMI category
Reported high cholesterol Reported high blood pressure Reported high blood sugar Smoking status Alcohol consumption Physical activity level |
| Population Projection | |
| Demographics | Age
Sex |
| Health Risk Factor and Disease Transition Modelling | |
| Risk Factors | BMI
Total cholesterol Systolic blood pressure Smoking status |
| Chronic Illness | Diabetes incidence
Heart disease events Stroke events |
| Mortality | CVD deaths |
| Outcomes | |
| Health Outcomes | YLL (Years of life lost)
DALY |
| Expenditure | Intervention costs
Health System costs |
| Scenario Comparator | ICER (Incremental cost effectiveness ratio) |
2.1 Base population
NCDMod is based on the 2005 National Health Survey (NHS05) (Australian Bureau of Statistics, 2006). The 2005 ABS National Health Survey is the legacy basefile from HealthAgeingMod (Walker et al., 2013). It is a cross-sectional, nationally representative confidentialised record file (CURF). It is part of the series of regular population health surveys run by the ABS designed to obtain national benchmark information on a range of health-related issues and to enable the monitoring of trends in health over time for Australia. The survey was conducted in the 10 months between August 2004 and June 2005 and included 25,906 interviews of non-institutionalised persons across Australia (excluding sparsely settled regions) (Australian Bureau of Statistics, 2006). The NHS05 provides a rich data source about the health of Australians including health status, chronic diseases, health risk behaviours and socio-demographic characteristics. The model’s basefile was reweighted to represent the more current 2010 Australian population. Reweighting is described more fully in Section 2.5. To facilitate simulation of the chronic diseases, additional refinement of the basefile was required. The basefile enhancements included:
Converting age into single years, via Monte Carlo simulation to allocate an age within the known five year age group, proportions are based on the ABS estimated resident population (ERP) 2010 (Australian Bureau of Statistics, 2015a);
BMI groups converted to continuous values, by randomly allocating a value in the known BMI group as per the modelling described for HealthAgeingMod (Walker et al., 2013);
Blood pressure categories converted to continuous values for systolic blood pressure. Those with elevated blood pressure were modelled separately from those with normal blood pressure. The models were from HealthAgeingMod (Walker et al., 2011; Walker et al., 2013) for detail of development). The models were developed from the Australian Diabetes, Obesity and Lifestyle Study (AUSDIAB) 2000 (Dunstan et al., 2001). The elevated blood pressure model used age, gender, BMI and exercise level as independent variables. The normal blood pressure model used age, gender, BMI, high cholesterol indicator, exercise level, smoking status and education level;
Imputation of having parental history of diabetes or not, based on AUSDIAB, using proportions by age group (13 categories) to allocate with Monte Carlo simulation;
Imputation of presence of left ventricular hypertrophy used logistic regression and Monte Carlo simulation. Independent variables used in the statistical model were age, gender, BMI and systolic blood pressure values;
Alignment of ethnicity with the definition on the Australian type 2 diabetes risk assessment tool (AUSDRISK) (Chen et al., 2010); by randomly selecting 33 per cent of those whose ethnicity was non-Australian to represent the “Southern European, Asian, and Aboriginal and Torres Strait Islanders” group in AUSDRISK;
Imputation of total cholesterol continuous value was modelled using the ABS Australian Health Survey (AHS) 2011. Due to changes in the survey methodology between 2005 and 2011, it was decided that the 2011 data offered the best reflection of cholesterol value distribution in the Australian population. There were separate models for those with high cholesterol and those with normal cholesterol. The independent explanatory variables used included age, gender, BMI, smoking status, elevated blood pressure and type 2 diabetes status; and
Imputation of high density lipoprotein (HDL) cholesterol value was based on AHS 2011 (Australian Bureau of Statistics, 2012). Independent variables used included age, gender, smoking status, exercise level, BMI and total cholesterol level.
For children in the base population who would become adults (that is, reach an age of 20 years) in the projection time period, base adult values needed to be imputed for the following variables:
Education level using logistic regression modelling to determine probability of having tertiary education and Monte Carlo simulation to allocate the outcome. Independent variables used were gender and an obesity indicator;
Exercise status was allocated the average number of minutes of exercise by gender for the 18–24 years olds on AHS 2011;
Cholesterol level was allocated the value of 5.5 mmol/L as per HealthAgeingMod (Walker et al., 2013);
Systolic blood pressure was allocated the normal value of 120 mmHg as per HealthAgeingMod (Walker et al., 2013);
BMI value was randomly imputed in proportion to BMI group distribution on AHS 2011 for 18–24 year olds. There was separate allocation for males and females. BMI values were then randomly allocated within the group that the records had been assigned; and
Known type 2 diabetes status random allocation based on AHS 2011 prevalence rate of 18–24 year olds (0.5%).
These children in the basefile at the start of the projection are important and included in the model to provide the records for the young adults in later projection years (that is, 2015, 2020 and 2025). On average, this group as they reach the 20–25 year old age group in the project were found to have similar attributes to the 20–25 year olds in the baseline dataset, though with less variability.
2.2 Cloning
To address any bias in the Monte Carlo simulation impacting on the model output due to the wide range of population weights, cloning of survey records was done so that a record’s population weight was no more than 20. The original basefile has a wide range of survey weights from 60 to almost 6,000. Due to our interest in some of the sub-populations with larger weights, we cloned the records to make the weights relatively even and ensure that selection of records with large weights was not unduly affecting the simulation estimates. The cloning created a basefile with 1,147,999 records that had population weights ranging between 0.01 and 20.
2.3 Risk factor and chronic disease incidence
The statistical transition models used within NCDMod were either sourced from literature on previously studied transitions such as Framingham risk equations for acute myocardial infract, stroke and cardiovascular deaths (Anderson, Odell, Wilson, & Kannel, 1991). In some instances, in-house modelling was undertaken, much of it based on the AUSDIAB data. The AUSDIAB baseline study undertaken in 1999–2000 was a cross-sectional, national, population-based survey, with a complex stratified cluster sampling design involved 11,247 adults aged 25 years and over. Follow-up studies were completed in 2005 and 2011. A detailed description of the survey methods have been published elsewhere (Barr et al., 2006; Dunstan et al., 2001; Tanamas et al., 2013).
Total cholesterol trajectory for individuals not receiving cholesterol treatment was modelled using equations from analysis by Wilson et al. (1994). The equation models change in total cholesterol over time using explanatory variables of change in age and weight for the time period. Similarly, HDL cholesterol change was modelled using change in age and weight over the time period. Modelling occurs separately for males and females. Those receiving cholesterol treatment were assumed to have constant cholesterol levels. If in the projection period an individual’s total cholesterol is greater than 7.5 mmol/L then they may start cholesterol lowering medication. This was based on previous modelling for School for Public Health Research (SPHR) Diabetes Prevention Model (Breeze et al., 2015). It is assumed that there was a 65% uptake amongst those eligible based on analysis of compliance for the first five years of statin treatment for primary prevention in general clinical practice (Ward et al., 2007). If cholesterol lowering medication is commenced, then total cholesterol is assumed to decrease by 1.4 mmol/L as reported from meta-analysis by Ara et al. (2009) and then remain at that level for the rest of the projection period.
The systolic blood pressure trajectory for the individual not receiving blood pressure treatment was based on analysis by Wu et al. (1980). This equation models change in blood pressure over time based on initial systolic blood pressure and age. Modelling occurs separately for males and females. Those receiving blood pressure treatment were assumed to have a constant systolic blood pressure over the time they use medication. If an individual’s systolic blood pressure is 140 mmHg or greater, they are placed on antihypertensive medications. With the use of antihypertensive medication systolic blood pressure is assumed to be reduced by 8.4 mmHg (based on analysis by Wald et al. (2009)) and remain at that level for the rest of the projection period.
Change in BMI value over time was modelled based on AUSDIAB 00–05 using a linear regression model. Independent variables used included age, gender, total cholesterol, systolic blood pressure, smoking status, presence of known type 2 diabetes and education level. From AUSDIAB, individuals with known type 2 diabetes were defined as those survey respondents reporting that they had ever been told by a doctor or nurse that they have type 2 diabetes and they were taking diabetes medication (either insulin or tablets); or they had ever been told by a doctor or nurse that they have type 2 diabetes and their blood test result for fasting plasma glucose was greater than or equal to the cut off point for diabetes. Incidence of known type 2 diabetes status was modelled based on AUSDIAB 00–11 using a logistic regression model with random effects. Independent variables used in the model included age, gender, BMI, systolic blood pressure, education level, ethnicity, parental history of diabetes and total cholesterol. It is assumed that those with known diabetes in the base population will continue to have known type 2 diabetes across the projection period.
Incidence of myocardial infarct across the time was modelled using Framingham equations (Anderson et al., 1991). These models are based on a non-proportional hazards weibull accelerated failure time regression model (Anderson, 1991). Included in the myocardial infarct model as explanatory variables were age, gender, systolic blood pressure, smoking status, total cholesterol, HDL cholesterol, diabetes status, left ventricular hypertrophy plus various quadratic and interaction terms.
Incidence of stroke was also modelled using Framingham equations (Anderson et al., 1991). Included in the stroke model as explanatory variables were age, gender, systolic blood pressure, smoking status, total cholesterol, HDL cholesterol, diabetes status, left ventricular hypertrophy plus various quadratic and interaction terms. It is assumed that regardless of having previous self-reported CVD, all individuals could experience a heart attack and/or stroke in the projection period.
Deaths due to CVD were modelled using Framingham equations (Anderson et al., 1991). Included in the CVD deaths model as explanatory variables were age, gender, systolic blood pressure, smoking status, total cholesterol, HDL cholesterol, diabetes status, left ventricular hypertrophy plus various quadratic and interaction terms.
2.4 Health expenditure modelling
Total health expenditure focused on government expenditure (Commonwealth, State and Local) and was inclusive of health goods and services: hospitals (both public and private), primary health care (including medical services, dental services, other health practitioners, community health, public health, benefits paid pharmaceuticals and all other medications). Research and administrative expenditure were excluded. Health expenditure was modelled based on diabetes status, CVD event and BMI group.
Costs were based on a linear regression model with total health expenditure as the outcome given known type 2 diabetes status, CVD event, BMI status (3 levels) and age using AUSDIAB data. Previous analysis of AUSDIAB that had focused on the cost of obesity in Australia (Colagiuri et al., 2010) was used as the basis for this analysis. The AusDiab 2005 survey included questions on the use of health services and health-related expenditure for the previous 12 months. Direct health care costs were deemed to include ambulatory services, hospitalisation, prescription medication and some medically related consumables. Costing data for medical services and diagnostics was based on the Medicare Benefits Schedule. Costs of medications were based on the Schedule of Pharmaceutical Benefits and modelled for out of pocket costs. The hospital costs were based on hospital bed day costs determined using Australian Institute of Health and Welfare (AIHW) hospital costs data.
Prices for medicines were adjusted to reflect government costs plus out of pocket charges and hospital bed days were calculated using the AIHW data (Australian Institute of Health and Welfare, 2015b).
2.5 Population projections
To account for the population growth, we used the ABS population projections (series B assumptions) (Australian Bureau of Statistics, 2013b). We used population projections to 2025 for Australians aged 20 years and over by five year age group and sex.
2.6 Reweighting
The NCDMod dataset provides socio-demographic information, including health conditions and economic characteristics for the Australian population for the year 2010 and then for every five years up to 2025 (that is, for 2010, 2015, 2020, and 2025). Changes in the demographic structure of the population (such as ageing), from 2005 to 2010 (and other modelled years to 2025) were captured through static ageing techniques. The NHS05 was weighted by the ABS to address the issue of unequal probability of individual selection in the survey, and to make the survey data a true representation of the Australian population in the survey year (Australian Bureau of Statistics, 2006). A survey weight designed to take into account the individual’s probability of selection and the clustering and the stratification of the sample was assigned to each record in the dataset. This weight reflects the number of people with similar characteristics in the Australian population at the survey year. Starting with these sample weights, we then reweighted the NHS05 to reflect the profile of the population aged 20 years and over in 2010 and other modelled years (2015, 2020, 2025) using a generalised regression reweighting algorithm programmed in a SAS macro called GREGWT. This macro was developed by the ABS and is commonly used to reweight their survey data (Bell, 2000). GREGWT uses the generalized regression method to modify initial survey weights so that the weighted totals match the externally provided totals known as benchmarks. It allows up to 30 benchmark datasets (Bell, 2000).
Population projections from the ABS (Australian Bureau of Statistics, 2013b) were used as benchmarks for population for Australians aged 20 years and over. The following projected populations were used as benchmarks in creating the 2010 basefile:
Population by age group and sex;
Number of individuals with diabetes by age group;
Number of individuals who are obese by age group and sex;
Number who currently smoke by age group;
Number of individuals who have hypertension by age group;
For the projections to 2015, 2020 and 2025 the population by age group and sex was used for benchmarking to account for expected population ageing and migration.
2.7 Validation
The model’s outputs were assessed to determine if the model output is reasonable for our purposes. Validation activities included debugging via code walk through and tracing of records to ensure that the model did not have obvious construction and syntax errors, model specification followed by clinical review for face validity, checking the model’s output plausibility and output checking against external data where available. Comparisons were made between the model base file of 2010 and the ABS AHS 2011 which was the closest Australian representative survey with respect to time that covered health topics. Outputs from the first projection period of the model 2015 were compared to the 2014/15 ABS National Health Survey, which provided guidance with respect to the quality of the transition equations and their interactions. The decision was taken by the research team (that included experienced modellers and clinicians) before commencing the validation that results within 10 per cent of the survey estimates (which themselves are subject to error) would be deemed acceptable.
3. Results
The key baseline characteristics of NCDMod for 2010 are presented in Tables 2 and 3 by gender. The database represented an Australian population of almost 17 million people, 48 per cent being male. The mean age of the population was 47.6 years with males being younger on average than females. Overall, 27 per cent of the population were obese, with the population estimated to have a mean BMI of 27.4 kg/m2. Just over six per cent of the population were estimated to have known type 2 diabetes. With respect to CVD, it was estimated that 2.3 per cent of the population reported ever having a heart attack and 1.5 per cent reported ever having a stroke. The estimated mean systolic blood pressure was 128.7 mmHg and the estimated mean total cholesterol was 5.6 mmol/L.
NCDMod – Estimated Australian Population Baseline Demographic and Disease Characteristics, 20 years and over, 2010.
| 2010 Baseline Characteristics | Gender | ||
|---|---|---|---|
| Obese | |||
| Male (%) | Female (%) | Total (%) | |
| BMI < 30 kg/m2 | 72.0 | 73.6 | 72.8 |
| BMI ≥ 30 kg/m2 | 28.0 | 26.4 | 27.2 |
| Known T2DM | |||
| Known T2DM | 5.7 | 6.7 | 6.3 |
| Not | 94.3 | 93.3 | 93.7 |
| Ever had a heart attack | |||
| Yes | 3.3 | 1.4 | 2.3 |
| No | 96.7 | 98.6 | 97.7 |
| Ever had a stroke | |||
| Yes | 1.6 | 1.4 | 1.5 |
| No | 98.4 | 98.6 | 98.5 |
| Overall | 100.0 | 100.0 | 100.0 |
| Total Population (in thousands) | 8,194 | 8,764 | 16,958 |
-
Source: NCDMod version June 2016.
-
Notes: BMI = Body mass index; T2DM = Type 2 diabetes mellitus.
NCDMod – Estimated Australian Population Baseline Distributional Characteristics, 20 years and over, 2010.
| Baseline Distribution | Gender | ||
|---|---|---|---|
| Male | Female | Total Population | |
| Age 2010 (in years) | |||
| Mean | 46.5 | 48.7 | 47.6 |
| Median | 45.0 | 47.0 | 46.0 |
| Standard Deviation | 77.29 | 82.10 | 79.97 |
| BMI2010 (kg/m2) | |||
| Mean | 27.9 | 26.9 | 26.4 |
| Median | 27.1 | 25.4 | 26.4 |
| Standard Deviation | 25.91 | 29.02 | 27.65 |
| Systolic Blood Pressure 2010 (mmHg) | |||
| Mean | 130.0 | 127.4 | 128.7 |
| Median | 125.8 | 121.0 | 123.7 |
| Standard Deviation | 56.86 | 74.51 | 66.84 |
| Total Cholesterol 2010 (mmol/L) | |||
| Mean | 5.5 | 5.6 | 5.6 |
| Median | 5.4 | 5.5 | 5.4 |
| Standard Deviation | 2.66 | 2.53 | 2.60 |
-
Source: NCDMod version June 2016.
-
Notes: BMI = Body mass index.
Some of the NCDMod key baseline characteristics were compared with the 2011 AHS (see Table 4) to validate the values achieved by reweighting the 2005 basefile. On these key characteristics, all were within ten per cent of the AHS values. It had been decided by the research team, which included experience modellers and clinicians that this would be regarded as acceptable variance in disease rates and risk factor levels as the low proportions being estimated mean even a small variance in the value results in a large percentage difference.
Comparison of NCDMod Baseline Characteristics with AHS 2011 values.
| Population Characteristics | NCDMod | AHS | % Difference |
| % 65 years and over | 19.4 | 17.8 | 9.0 |
| % male | 48.3 | 49.4 | -2.2 |
| % type 2 diabetes (self-reported) | 6.3 | 5.8 | 8.6 |
| % obese (BMI ≥ 30 kg/m2) | 27.2 | 28.8 | -5.6 |
| Population Size | 16,957,458 | 16,393,424 | 3.4 |
-
Source: NCDMod version June 2016.
-
Notes: BMI = Body mass index; AHS = Australian Health Survey 2011.
Tables 5 and 6 present the projected values of health indicators and health events estimated by NCDMod for the time period 2010 to 2025. In the projection it was estimated that mean BMI would continue to increase over time, as would the percentage of persons classified as being obese. Mean systolic blood pressure was estimates to increase over the projection period and total cholesterol held relatively constant. The rate of new type 2 diabetes cases was relatively constant between 2010 and 2020, with an increase in the period between 2021 and 2025. The number of disease events are presented in Table 5 are the sum of all events in the five year period. That is between 2011 and 2015 there were just over 261,000 new cases of known type 2 diabetes. This increased between 2016 and 2020 to just under 289,000 new cases of known type 2 diabetes and further increased to just over 325,000 new cases between 2021 and 2025. The rate of cardiovascular events and cardiovascular death had an increase, but that rate of increase was declining over time.
NCDMod Estimated mean Values of Health Indicators 2010–2025.
| Outcome | 2010 | 2015 | 2020 | 2025 |
| BMI (kg/m2) | ||||
| Total | 27.4 | 28.1 | 28.7 | 29.4 |
| Female | 26.9 | 27.7 | 28.4 | 29.2 |
| Male | 27.9 | 28.5 | 29.0 | 29.7 |
| SBP (mmHg) | ||||
| Total | 128.7 | 130.3 | 130.9 | 131.9 |
| Female | 127.4 | 129.0 | 129.9 | 131.2 |
| Male | 130.0 | 131.6 | 132.0 | 132.7 |
| Total Cholesetrol (mmol/L) | ||||
| Total | 5.6 | 5.6 | 5.5 | 5.4 |
| Female | 5.6 | 5.6 | 5.5 | 5.5 |
| Male | 5.5 | 5.5 | 5.5 | 5.4 |
-
Source: NCDMod version June 2016.
-
Notes: BMI = Body mass index; SBP = systolic blood pressure.
NCDMod Projected Health Events and Rates, 2011–2025.
| Variable | 2011–2015 | 2016–2020 | 2021–2025 |
|---|---|---|---|
| New Known Type 2 Diabetes | 261,496 | 288,503 | 325,301 |
| CVD Events (excl. CVD deaths) | 461,566 | 600,715 | 697,050 |
| Years Lived in Disability | 1,380,228 | 1,826,728 | 2,085,673 |
| CVD Deaths | 258,948 | 378,091 | 445,225 |
| Years of Life Lost | 2,527,629 | 3,276,962 | 3,669,757 |
| New Known Type 2 Diabetes Rate (per 100,000 population) | 287.6 | 285.0 | 296.3 |
| CVD Events (excl. CVD deaths) Rate (per 100,000 population) | 507.6 | 593.4 | 635.0 |
| CVD Deaths Rate (per 100,000 population) | 284.8 | 373.5 | 405.6 |
-
Source: NCDMod version June 2016.
-
Notes: CVD = cardiovascular disease.
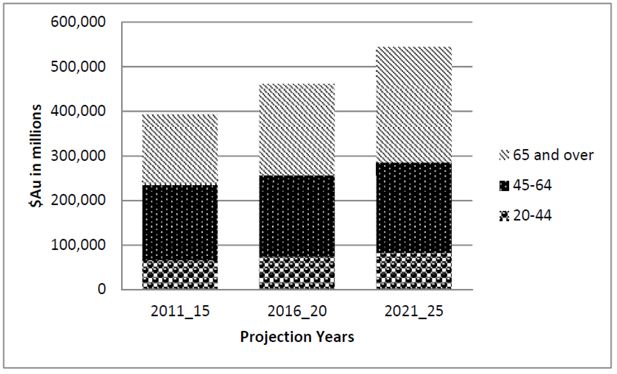
Figure 2 shows the health expenditure estimated by NCDMod for the time period 2011 to 2025 in five year groups. The projected total health expenditure increased from $AU 393,415 million in 2011–2015 to $AU544,513 million in 2021–2025, an almost 40 per cent increase. The expenditure in each time period increased with increased age, that is, there was more health expenditure on those in the oldest age groups. This was consistently seen in the projection.
Initial validation of the model has been completed. Table 7 illustrates the comparison of the NCDMod outputs for the end of the first time period that is 2015. There are three measures (percentage obese, percentage with measured high cholesterol and prevalence of known type 2 diabetes) that perform such that simulated values are within 10 per cent of the ABS survey data. Performance is less satisfactory for the indicators of percentage who ever smoked, percentage with high blood pressure and percentage with CVD. With these indicators it is worth noting that whilst the percentage difference is comparatively large the absolute percentage point difference is still small. This occurs particularly in the case of CVD prevalence because of the relatively small rates of the condition at a population level. Additionally, the level of health expenditure was compared to 2013/14 AIHW data on health expenditure which indicated that approximately $AU69 billion was spent on health services (excluding research and administration) for adults aged 18 years and over. This compares with our models estimate of $AU66.2 billion spent in 2015, an underestimate of approximately 4 per cent.
NCDMod 2015 Outputs Compared to ABS National Health Survey 2014/15.
| Population Characterstics | NCDMod 2015 | NHS 2014/15 | Absolute % point difference | %Difference |
|---|---|---|---|---|
| % Ever Smoke | 20.9 | 17.4 | 3.5 | 20.1 |
| % Obese (BMI ≥ 30 kg/m2) | 26.1 | 27.9 | 1.8 | -6.5 |
| % High Blood Pressure | 18.4 | 21.5 | 3.1 | -14.4 |
| % High Total Cholesterol | 34.3 | 32.8 | 1.5 | 4.6 |
| % T2DM | 5.5 | 5.1 | 0.4 | 7.8 |
| % CVD prevalence | 3.2 | 5.2 | 2.0 | -38.5 |
-
Source: NCDMod version June 2016 and ABS NHS 2014/15 (Australian Bureau of Statistics, 2015b).
-
Notes: Adults aged 18 years and over, aligning with ABS definitions used in reporting. T2DM = Type 2 diabetes mellitus. CVD = Cardiovascular disease.
Discussion
We have developed a microsimulation model called NCDMod to project the outcomes of interventions on chronic conditions, initially focused on diabetes and CVD, as well as obesity. NCDMod is able to capture the impacts of population ageing, and shifts in incidence of specific chronic diseases. NCDMod will be used to estimate, under given scenarios, (i) the incidence of diabetes and CVD; (ii) total health expenditure and specific cost of interventions being considered; and (iii) years of life lost and disability ability adjusted life years. Further chronic disease prevalence data under given scenarios can be linked to Health&WealthMod 2030 to estimate (i) the number of people out of the labour force due to their ill health; and (ii) the lost income and savings of people who have left the labour force because of their ill health, compared to those who continued in paid employment (Schofield et al., 2014). NCDMod will also be used to compare estimates of the potential medium-term health care cost savings from various health interventions that address these health conditions, and risk factors such as obesity and physical inactivity.
The 2010 basefile of the model has been validated against the 2011 NHS. Validation of the first projection period to 2015 was also done via comparison with the 2014/15 NHS. These surveys are the closest in time period to our model. The validation indicates a reasonable alignment of key characteristics between the survey and the model, with many model characteristics being within ten per cent of the survey measures. The results of this preliminary validation are promising, however there is a need for more validation studies. Future validation will include re-evaluation of the current input parameters, comparisons of model output with the actual trends observed in administrative and survey data as it becomes available, and sensitivity analyses.
This provides confidence in the robustness of using the model’s basefile for projection of outcomes out to 2025. The model currently simulates a number of chronic diseases associated with obesity to 2025. With the increasing emphasis on the impacts of obesity, the model will over time be expanded to account for other diseases with known links to obesity such as arthritis and pain. The model is focussed on direct health care costs. The linkage of this model, NCDMod with Health&WealthMod 2030 in future studies will allow productivity projections for adults aged 45–65 years, a unique extension of this modelling.
Australia’s increasing population and associated population ageing will increase the future demand for health care and in turn the outlay on health care. Health care spending has been steadily growing, from $AU 95 billion in 2003/04 to $AU 155 billion in 2013/14 (expressed as constant 2013/14 prices) (Australian Institute of Health and Welfare, 2015b). Australian Treasury projections estimate continued rises in health expenditure by the Commonwealth government to 5.5 per cent of GDP (gross domestic product) in 2054/55 (Commonwealth of Australia, 2015). Trends in chronic disease, co-morbidity and risk factors will also have substantial impact on need for health care and consequent health expenditure. Understanding if interventions that are shown to be effective in a clinical trial offer population level impacts if offered to the wider population and are cost-effective in the wider population setting are important in a context of fiscal sustainability. This model offers the potential to trial such scenarios without the expense of programme roll outs that may prove to be cost-inefficient.
There are several areas that we acknowledge limit conclusions that can be made from the model. Currently the model predominantly focuses on just two chronic diseases and their associated risk factors (with a major emphasis on obesity). Within the model there are other chronic diseases available on the health survey used for the basefile, such as arthritis and depression that could be readily incorporated into the modelling at a later stage. In the modelling of years of life lost, the scenario outcomes are a conservative estimate of the life years gained because the impacts through diseases other than diabetes and CVD are not accounted for in the model.
In using a household survey as the model’s basefile, the records only cover those people who live in households, those who are residing in non-private dwellings such as hostels or nursing homes at the time of the survey are not included. Consequently, those in the poorest health are effectively excluded from NCDMod. The result is that outputs from the model will be an underestimate of the scenario compared to modelling that included the institutionalised population.
Several of the transition equations have been sourced from the literature such as those to determine likelihood of CVD which were based on Framingham. Using such equations that were based on populations from another country with different levels of risk factors is problematic as evidenced by the validation. However, Framingham equations remain those recommended and endorsed for Australia in the 2012 National Health and Research Council guideline for calculation of absolute cardiovascular risk. We acknowledge that the values of the specific parameters in NCDMod are potentially subject to criticism and may need to be modified as new and better data become available.
A technical limitation of microsimulation models is the random variability present due to use of Monte Carlo simulation methods. That is, different runs of the model are expected to have slightly different outputs, even with the same parameters if using different random number seeds. This model, like many other health models, does not account for income and technology based changes in health expenditures. Whilst in recent times health technology has driven up the cost of health care, the impact of health care breakthroughs is highly uncertain. Issues that impact the cost implications of new health technology include its commercialisation, population level of uptake and secondary side effects.
The reliance on randomised clinical trial data may have limited generalizability to inform intervention outcomes in modelling the community/population impacts of the intervention. Clinical trials recruit a special group of people often highly educated and highly motivated, with a range of exclusion criteria, thus the outcomes of the intervention in a community setting amongst a more diverse group of people may not replicate the outcomes previously reported. Further, in the scaling of interventions to local areas there is the potential that the program is not implemented in the same manner as reported in the clinical trial. Again this may result in shifts in the level of outcome when the intervention is community based.
Results from NCDMod will help to fill gaps in current Australian evidence on the population level impacts of interventions to prevent/delay chronic health conditions particularly diabetes, heart disease and obesity. Using this model, we will be able to contribute to existing evidence on how clinical trial outcomes of interventions impact at a population level in Australian adults. The techniques used in NCDMod will ensure that policymakers are drawing on the most reliable estimates available of the medium-term health care costs and potential savings offered by a variety of health interventions including prevention, screening and treatment. Further, in combination with Health&WealthMod2030 the modelling will be able to offer evidence regarding the potential savings health interventions have on the long-term costs (both from an individual and government perspective) of ill health leading to unplanned retirement and the additional workers who may be able to continue to work due to delayed/prevented chronic disease.
A1.
Comparing and Contrasting NCDMOD With Healthageingmod.
| Model Element | HealthAgeingMod | NCDMod | ||
|---|---|---|---|---|
| Basefile | NHS 2005 | NHS 2005 | ||
| Cloning of Records | No | Yes | ||
| Number of records in basefile | Approximately 26,000 records | Approximately 1.15 million records | ||
| Basefile reweighting | No | SAS macro GREGWT (Bell, 2000) was used to reweight the basefile to 2010 based on benchmarks of ABS ERP 2010 in 5-year age group-sex numbers; ABS 2011 in 5- year age group-diabetes numbers, 5-year age group- obesity numbers, 5- year age group high blood pressure numbers and 5- year age group-smoker numbers. | ||
| Projection reweighting | Reweighted 2005 to 2010 using ABS population projections series B(Australian Bureau of Statistics, 2008) routinely. | Reweighted 2010 to 2015, 2020 and 2025 using ABS population projections series B (Australian Bureau of Statistics, 2013b) routinely. | ||
| Alignment | Alignment of CVD deaths according to the trend of ABS causes of death data 2000–2006, such that in 2005 there were approximately 35,000 CVD deaths (Walker et al., 2013) | Alignment of number obese by age-sex groups in 2015 using GREGWT and benchmarks from 2014/15 ABS NHS data. | ||
| Age: imputation of single years | Monte Carlo simulation with allocation across each single year within the 5 year age group, with 20% going into each year | Monte Carlo simulation by gender, with allocation across each year within the 5 year age group based on ABS ERP 2010 as the distribution of age within 5 year group. | ||
| Imputation of parental history of diabetes | No | Allocated by Monte Carlo simulation. Age based probability from AUSDIAB00. | ||
| Ethnicity | Based on NHS05 country of birth variable made binary Australian born or not. Additional flag of ethnicity to mark “Southern European, Asian, ATSI” is a random allocation of 0.33 those not “Australian born”. | |||
| Education level | Binary variable – post school or not based on NHS05 education data | Same as HealthAgeingMod. | ||
| BMI: imputation of continuous values | Imputed randomly using uniform distribution with 8 BMI bands on NHS05 | Same as HealthAgeingMod. | ||
| BMI transition | Models BMI at end of 5 year period using OLS: 3.225 – 0.021 * (AGE) -0.135 * HBA1C * HBA1C scale + 1.000 * BMIvalue – 0.005 * SBP – 0.147 * cholesterol + 0.129 * female Based on USDIAB 00–05 | Models BMI change across 5 year period: 2.694 – 0.022 * (aget+1) + 0.151 * sex -0.047 * cholesterol -0.005 *SBP + 0.192 * smoker -0.354 * diab2 -0.092 * ED level
Based on AUSDIAB 00–05. |
||
| Smoking status transition | Nil | Models smoking status at end of 5 year period using logistic regression to determine probability.
If smoker: 1.429 – 0.012 * age10 -0.012 * male +0.092 * EDlevel If non-smoker: 2.116 + 0.056 * age10 -0.010 * male -0.372 * EDlevel Monte Carlo simulation used to allocate state. |
||
| Total cholesterol: impute continuous value | OLS modelling to allocate a total cholesterol value.
If high cholesterol: 5.339 + 0.002 * AGE + 0.012 * BMI value + 0.048 * hba1c Value + 0.003 * BP value -0.008 * ED level If normal cholesterol: 4.038 + 0.005 * AGE + 0.012 * BMI value -0.036 * hba1c Value + 0.002 * BP value -0.037 * Exercise_3+0.005 * ED level Based on AUSDIAB 2000. |
If self-reported high cholesterol:
Exp(1.635 – 0.0026*male + 0.003 * age + 0.007 * BMI value -0.0001 * BMIvalue2 + 0.007 * smoke + 0.015 * HB -0.003 * diabetes). If not self-reported high cholesterol: Exp(1.262 + -0.028*male + 0.001 *age + 0*age2 + 0.023 * BMI value -0.0003 * BMI value2 + 0.032 * smoke + 0.039 * High BP -0.206 * diabetes) Based on AHS2011 data. |
||
| HDL Cholesterol: impute continuous value | No | Modelled using OLS with exponential transformation: Exp(0.599 + 0.001*age – 0.088 * male -0.074 * smoker + 0.033 * e3 -0.016 * BMI value + 0.036 * Cholesetrol value + 0.040 * male_smoke – 0.004*male_bmi). | ||
| Systolic blood pressure: impute continuous variable | If High BP: 128.185+0.346*AGE + 1.007*female + 0.139*BMI value+1.665*E1
If normal BP: 99.183+0.212*AGE-5.521*female+0.582*BMI value+1.153*Hi Cholesterol – 0.749*Exercise_2-1.093*SMOK- 0.071*ED level Based on AUSDIAB 2000. |
Same as HealthAgeingMod. | ||
| Systolic blood pressure transition | Model SBP at end of 5 year period: 23.551 + 0.201*(AGE)+0.437*BMI value * BMI scale +0.618 *BP value * BP scale – 2.703 * female
Based on AUSDIAB 00–05. |
Annual change in SBP modelled as:
If aged less than 35 years there is no change. If female aged 35 and over: 35–45 years. :2.445+0.107*(SBP -117.891 45–55 years : 2.278 +0.039*(SBP -127.312) 55–65 years :2.052+- 0.003*(SBP -137.656); 65y.o.+ : 2.296 + 0.024*(SBP -125.177); If male aged 35 and over: 35–45 years: 1.321 + 0.015*(SBP -124.825); 45–55 years: 1.1915 + 0.064*(SBP -127.948); 55–65 years: 2.860 + 0.058*(SBP -128.675); 65 years + : 1.85 + 0.048*(SBP-126.722); Based on Wu et al. (1980). If on antihypertensive medication then SBP remains unchanged. |
||
| Systolic blood pressure medication | Nil | If SBP greater than 160 allocated to start antihypertensives. | ||
| Diabetes duration | Allocated such that:
If 35<=AGE<55 then duration is 7.5 years If 55<=AGE<65 then duration is 10 years if aged 65 years and over then duration is 15 years |
Same as HealthAgeingMod. | ||
| Impute has undiagnosed diabetes | Monte Carlo simulation amongst those without diabetes
Probability based on logistic regression model: -29.242+0.038*AGE-0.073*female+3.783*hba1c Value+0.030*BMI value +0.021*BP value-0.048*Hi Cholesterol -0.164*E1- 0.143*Exercise_2-(-0.164- 0.143)*Exercise_3 – 0.057*SMOK+0.070*ED level |
Same as HealthAgeingMod. | ||
| Transition to self- reported diabetes | Logistic regression model: – 23.200 – 0.020*(AGE) +0.835*female + 3.344*hba1c + 0.041*BMI + 0.011*SBP +0.403*SMOK
Based on AUSDIAB Same as HealthAgeingMod. |
|||
| Transition to known diabetes | Logistic regression model: – 28.826 + 3.887 * hba1c + 0.078 * BMI + 0.015 * SBP Based on AUSDIAB | Random effects model of probability develop known diabetes across 5 year period:
-9.429 -0.063 * age10 – 0.717 * sex + 0.022 * BMI + 0.015 * SBP -0.449 * ed level – 0.657 * ethnic + 0.092 * previous Hx Diab – 0.344 * total cholesterol + 0.005 * age * bmi + 0.841* sex * previous Hx Diab Based on AUSDIAB00-05-11. |
||
| Year diabetes commenced | Random allocation so 50% in year 2 and 50% in year 4 of five year transition period. | Random allocation into single years across the 5 year period. | ||
| Impute has IFG | Monte Carlo simulation amongst those without diabetes or undiagnosed diabetes.
Probability based on logistic regression model : -15.915 + 0.017*AGE-0.947 * female + 2.172 * hba1c Value + 0.063 * BMI value -0.003 * BP value – 0.111 * Hi Cholesterol – 0.027 * Exercise_1 + 0.064 * Exercise_2-(-0.027+0.064) * Exercise_3 -0.109 * SMOK + 0.038 * ED level |
Same as HealthAgeingMod. | ||
| Impute pre-diabetes IGT | ||||
| Monte Carlo simulation amongst those without diabetes or undiagnosed diabetes.
Probability based on logistic regression model : -16.650 + 0.029 * AGE + 0.308 * female + 1.924 * hba1c Value + 0.050 * BMI value + 0.014 * BP value – 0.031 * Hi Cholesertol-0.094 * Exercise_1 – 0.087 * Exercise_2-(- 0.094 * E1 – 0.087) * Exercise_3 – 0.065 * SMOK -0.138 * ED level |
Same as HealthAgeingMod. | |||
| Life expectancy to calculate YLL | By gender single years based on Australian Government Actuary Life Tables 2005–07 | By gender single years based on ABS life tables 2010–12. | ||
| HbA1c impute continuous value | If has self-reported high sugar model hba1c Value = 7.172 -0.0235* AGE + 0.013 * BP value – 0.408 *
Hi Cholesterol If self-report not having high sugar levels then hba1c Value = 4.455 + 0.007 * AGE -0.070 * female + 0.0113 * BMI value +0.0003 * BP value + 0.032 * Hi Cholesterol + 0.035 * Exercise_1 + 0.029 * Exercise_2 + 0.013 * SMOK -0.004. |
Same as HealthAgeingMod. | ||
| HbA1c transition | OLS to calculate the new HbA1c value at the end of 5 year projection 1.545 + 0.002 * (AGE in 2010) + 0.691 * HBA1C value + 0.008 * BMI value
Based on AUSDIAB 00–05. |
Same as HealthAgeingMod. | ||
| Impute Left Ventricular Hypertrophy (LVH) status | Nil | Logistic regression model to model probability: -7.167 + 0.054 * age + 6.043 * male -0.156 * BMI value + 0.027 * BP value- 0.075 * male_age Based on AUSDIAB 05. Monte Carlo simulation to allocate condition. | ||
| CVA incidence | Logistics regression model: -9.550 + 0.050 * AGE + 0.027 * BMIvalue
Based on AUSDIAB 00–05. Monte Carlo allocation of events. |
Non-proportional hazards Weibull accelerated failure time model to calculate probability of CVA event: 26.512 + 0.202 * female – 2.374 * log(age) -2.464 * log(SBP) – 0.391 * SMOK -0.023 * log(total chol/HDL) -0.309 * diab2 – 0.263 * female * Diab2 – 0.236 * LVH
Based on Framingham ( Anderson et al., 1991). Monte Carlo simulation to allocate event |
||
| Allocate year of CVA incident | Random allocation so 50% in year 2 and 50% in year 4 of five year transition period. | Random allocation into single years across the 5 year period | ||
| Heart disease incidents | Probability of event in 5 year period using logistic regression model: -10.021 + 0.046 * AGE – 1.031 * female + 0.051 * BMI + 0.016 * SBP – 0.478 * CVD history + 0.346 * ED level Based on AUSDIAB 00–05. Monte Carlo allocation of events | Non-proportional hazards Weibull accelerated failure time model: 11.471 + 10.511 * female – 0.797 * log(age)-5.422 * log(age)*female + 0.710 * log(age)*log(age)*female – 0.662 * log(SBP)- 0.268 * SMOK -0.428 * log(total chol/HDL)-0.153 * diab2 -0.117 * female * diab2 -0.159 * LVH*male;
Based on Framingham (Anderson et al., 1991). Monte Carlo simulation to allocate event |
||
| Allocate year of heart disease event | Random allocation so 50% in year 2 and 50% in year 4 of five year transition period. | Random allocation into single years across the 5 year period | ||
| CVD deaths | Used Anderson (1991) Equation. Adjustment of population weights to reflect total population after these records removed for the next time period due to their “death”. | Used Anderson(1991) Equation to flag those records to reflect the deaths in the 5 year transition period. The records are reused with the population weights to reflect the whole population for the end of transition period | ||
| DALY weights | Used Begg et al. (2007) and Lopez et al. (2006) as Source. | Used GBoD study 2010 (Salomon et al., 2012) as basis of estimates | ||
| Imputation of children’s risk factors i.e. the records that become adults across the projection period | Imputes BMI to new 18+ year olds in proportion to NHS 2005 distribution of BMI categories for 18–19 years. Individual given mid- point for continuous value of BMI Total Cholesterol level allocated as 4.7
HbA1c allocated as 4.8 Systolic blood pressure allocated as 120 |
BMI imputed by gender, allocate BMI category based on distribution of AHS 2011. Then randomly allocated continuous variable using uniform distribution across group BMI band they in which they were allocated. Allocated exercise as 180 minutes for boys and 140 minutes for girls
Used ABS AHS 2011 age 18–34 years with 0.5 prevalence of diabetes to allocate T2 diabetes Future adult education was randomly allocated using probabilities from logistic regression model :-1.347 + 0.033*sex + 0.651 *obese Rest of risk factors as per HealthAgeingMod. |
||
| Annual disease costs | Models the direct health costs associated with diabetes and CVD incidents. Both the cost of diabetes and the cost of CVD were Sourced from the literature. Persons with both diabetes and a CVD event in the time period had the costs added together and given 20% extra cost.
Direct health costs based on if has diabetes and/or CVD. Costs Sources mainly from Clarke et al. (2008) 0.20 factor added to those with both CVD and diabetes. |
Based on AUSDIAB 05 for health service usage and costs based on MBS, PBS and AIHW hospital costs data. The equation was estimated using a linear regression model. The predictive variables included were: BMI, diabetes status and CVD status. This method provides a cost across the complete Australian population, calculating individual annual health system costs: 7599.91 + 3112.04*diab2 + 9330.60*CVD – 1830.25*BMI_normal – 1456.55*BMI_overweight – 4762.96 * age25 -3141.65 * age45 | ||
| Language/software used to write the code and run the scenarios SAS v9.2 | SAS v9.4 |
References
-
1
A Nonproportional Hazards Weibull Accelerated Failure Time Regression ModelBiometrics 47:281.https://doi.org/10.2307/2532512
- 2
-
3
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluationHealth Technol Assess. 13:1–74–75–118.https://doi.org/10.3310/hta13340
-
4
National Health Survey: Users’ Guide -Electronic Publication, 2004-05 Vol. ABS Cat. No. 4363.0.55.001National Health Survey: Users’ Guide -Electronic Publication, 2004-05 Vol. ABS Cat. No. 4363.0.55.001.
-
5
3222.0 -Population Projections, Australia, 2006 to 2101. In ABS (Series Ed.) Vol. ABS Cat. No. 3222.03222.0 -Population Projections, Australia, 2006 to 2101. In ABS (Series Ed.) Vol. ABS Cat. No. 3222.0.
-
6
Australian Health Survey: Users’ Guide, 2011-13 Vol. Cat No. 4363.0.55.001Australian Health Survey: Users’ Guide, 2011-13 Vol. Cat No. 4363.0.55.001.
-
7
Australian Health Survey: Updated Results, 2011-12. ABS Vol. ABS Cat. No. 4364.0.55.003Australian Health Survey: Updated Results, 2011-12. ABS Vol. ABS Cat. No. 4364.0.55.003.
-
8
Population Projections, Australia, 2012 (base) to 2101 Cat No. 3222.0 Vol. Cat No. 3222.0Population Projections, Australia, 2012 (base) to 2101 Cat No. 3222.0 Vol. Cat No. 3222.0.
-
9
Australian Demographic Statistics, Mar 2015 Vol. ABS Cat. No. 3101.0Australian Demographic Statistics, Mar 2015 Vol. ABS Cat. No. 3101.0.
-
10
National Health Survey: First Results, 2014-15 Vol. Cat No. 4364.0.55.001National Health Survey: First Results, 2014-15 Vol. Cat No. 4364.0.55.001.
-
11
Australia’s Health 2014. Australia’s Health Series No. 14. Cat. No. AUS 178. Vol. Australia’s Health Series No. 14. Cat. No. AUS 178Australia’s Health 2014. Australia’s Health Series No. 14. Cat. No. AUS 178. Vol. Australia’s Health Series No. 14. Cat. No. AUS 178.
-
12
Health-Care Expenditure on Cardiovascular Diseases 2008–09 Cat. No.CVD 65Health-Care Expenditure on Cardiovascular Diseases 2008–09 Cat. No.CVD 65.
-
13
Cardiovascular disease, diabetes and chronic kidney disease—Australian facts: Risk factors. Cardiovascular, diabetes and chronic kidney disease series no. 4. Cat. no. CDK 4Cardiovascular disease, diabetes and chronic kidney disease—Australian facts: Risk factors. Cardiovascular, diabetes and chronic kidney disease series no. 4. Cat. no. CDK 4.
-
14
Health expenditure Australia 2013–14. Health and welfare expenditure series no.54. Cat. no.HWE 63Health expenditure Australia 2013–14. Health and welfare expenditure series no.54. Cat. no.HWE 63.
- 15
-
16
The Burden of Disease and Injury in Australia 2003. PHE 82 Vol. PHE 82The Burden of Disease and Injury in Australia 2003. PHE 82 Vol. PHE 82.
-
17
Weighting and Standard Error Estimation for ABS Household Surveys. Australian Bureau of Statistics Methodology Advisory Committee PaperWeighting and Standard Error Estimation for ABS Household Surveys. Australian Bureau of Statistics Methodology Advisory Committee Paper.
-
18
School for Public Health Research (SPHR) Diabetes Prevention Model: Detailed Description of Model Background, Methods, Assumptions and Parameters Health Economics & Decision Science (HEDS). Discussion Paper SeriesSchool for Public Health Research (SPHR) Diabetes Prevention Model: Detailed Description of Model Background, Methods, Assumptions and Parameters Health Economics & Decision Science (HEDS). Discussion Paper Series.
-
19
Simulating the Need for Health-and Elderly Care in Sweden – A Model Description of SESIM-LEVIn: G Dekkers, M Keegan, C O’Donoghue, editors. New Pathways in Microsimulation. Ashgate. pp. 41–60.
- 20
-
21
AUSDRISK: an Australian Type 2 Diabetes Risk Assessment Tool based on demographic, lifestyle and simple anthropometric measuresMed J Aust 192:197–202.
-
22
A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68)Diabetologia 47:1747–1759.
-
23
Estimating the cost of complications of diabetes in Australia using administrative health-care-dataValue in Health 11:199–206.
- 24
- 25
- 26
-
27
Projections of Population, Education, Labour Supply and Public Pension BenefitsSocial and Economic Studies, 101.
-
28
Projection of Social Burden of the Elderly in Japan Using INAHSIM-IIEpidemiology Research International 2012.
-
29
The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysisBMC Public Health, 9, 88.
-
30
UKPDS outcomes model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study: UKPDS 82Diabetologia 56:1925–1933.
-
31
Stroke and active life expectancy in the United States, 1999–2009472–477, Stroke and active life expectancy in the United States, 1999–2009, Disability and Health Journal, 7, 4.
-
32
The Cost of Diabetes in Adults in AustraliaDiabetes Research and Clinical Practice 99:385–390.
-
33
Global and regional burden of disease and risk factors, 2001: systematic analysis of population health dataLancet 367:1747–1757.
-
34
More than just population ageing : an evaluation using dynamic microsimulation of the escalation of Australian government expenditure on health over the next 40 years
-
35
Projections of preventable risks for cardiovascular disease in Canada to 2021: a microsimulation modelling approachCMAJ Open 2:E94–E101.
-
36
CAPP_DYN: A Dynamic Microsimulation Model for the Italian Social Security System. Department of Economics 0595, University of Modena and Reggio E., Faculty of Economics "Marco Biagi"
-
37
Future modelling of chronic diseases: foresight and beyondThe Lancet, 380, 9, 10.1016/S0140-6736(13)60365-7.
-
38
Computer Modeling of Diabetes and Its Complications: A Report on the Fifth Mount Hood Challenge MeetingValue in Health 16:670–685.
- 39
-
40
Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010Lancet 380:2129–2143.
-
41
Labour force participation and the influence of having CVD on income poverty of older workersInternational Journal of Cardiology 156:80–83.
-
42
Lost productive life years caused by chronic conditions in Australians aged 45–64 years, 2010-2030Med J Aust. 203:260.
-
43
Health&WealthMOD2030: A microsimulation model of the long term economic impacts of disease leading to premature retirements of Australians aged 45-64 years oldInternational Journal of Microsimulation 7:94–118.
-
44
Development, validation, and application of a microsimulation model to predict stroke and mortality in medically managed asymptomatic patients with significant carotid artery stenosisValue Health 10:489–497.
- 45
-
46
Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trialsAm J Med. 122:290–300.
-
47
Cost-benefit model system of chronic diseases to assess and rank prevention and treatment options-HealthAgeingMod. Australian Centre for Economic Research on Health Research Report No 10Cost-benefit model system of chronic diseases to assess and rank prevention and treatment options-HealthAgeingMod. Australian Centre for Economic Research on Health Research Report No 10.
-
48
Health Policy in Ageing Populations: Economic Modeling of Chronic Disease Policy Options in AustraliaNetherlands: Bentham Science Publishers.
-
49
A systematic review and economic evaluation of statins for the prevention of coronary eventsHealth Technol Assess 11:1–160.
-
50
Determinants of Change in Total Cholesterol and HDL-C With Age: The Framingham StudyJournal of Gerontology 49:M252–M257.
-
51
The economic burden of obesity worldwide: a systematic review of the direct costs of obesityObesity Reviews 12:131–141.
-
52
Obesity: Preventing and managing the global epidemic. WHO technical report series. Report of a WHO ConsultationObesity: Preventing and managing the global epidemic. WHO technical report series. Report of a WHO Consultation.
-
53
On the relation between blood pressure change and initial valueJournal of Chronic Diseases 33:637–644.
Article and author information
Author details
Acknowledgements
The development and application of the microsimulation model outlined in this paper, NCDMod, is funded by the NHMRC Program Grant (under grant APP1037786).
Publication history
- Version of Record published: December 31, 2016 (version 1)
Copyright
© 2016, Lymer et al.
This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.